High-performing Health Systems: Closing the Chasm between Good Policy Intent and Real Service Transformation
- Leanne Wells

- Nov 2, 2024
- 7 min read
Updated: Dec 11, 2024
AUSTRALIAN PRIMARY HEALTH CARE INSIGHTS AND INNOVATION SERIES
Leanne Wells and Paresh Dawda
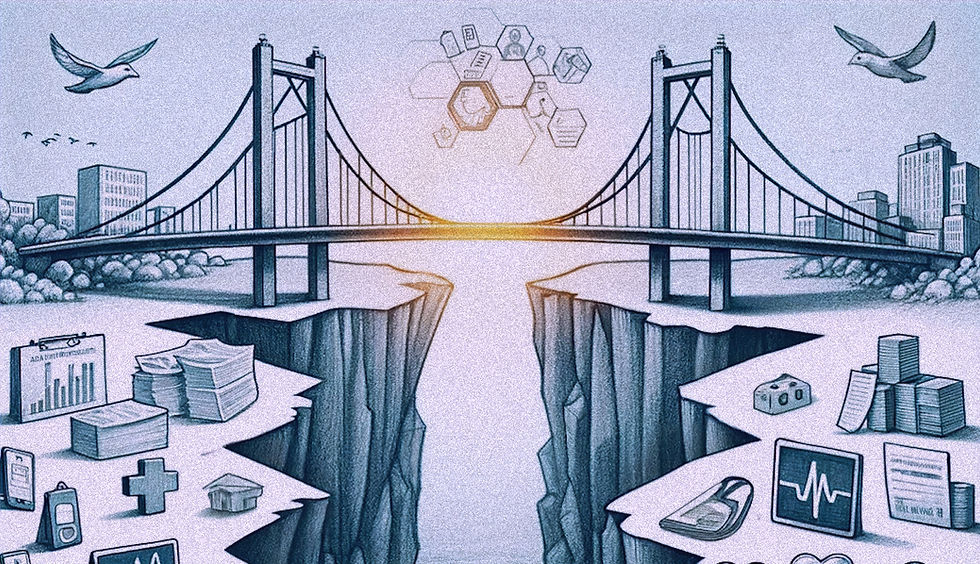
Healthcare systems are challenged to better cater for contemporary demands at the same time as recovering from the aftershocks of COVID-19. The need to disrupt healthcare and put it on a sustainable footing is the subject of intense policy discourse and never far from the headlines.
No country is doing well
Several new reports paint a sobering picture about what’s ailing health care and of societies in distress. They reinforce that accessible primary care is the backbone of high-performing health systems, yet all point to a crisis in primary care.
In the UK, Lord Darzi’s review of the NHS and the IPPR Commission on Health and Prosperity report that health challenges have reached “historic proportions” helping to trigger Change NHS “the biggest ever conversation about the future of the NHS”.
Australia’s high-profile Strengthening Medicare Taskforce has laid out the most pressing investments needed in primary care. A series of subsequent reviews propose an ambitious new funding architecture for primary care practices, among other areas of policy shift.
In Canada, the public has been their guide using strategies such as citizen panels to develop an Our Care Standard to assess the adequacy of primary care.
Mirror, Mirror 2024, the Commonwealth Fund’s comparisons of health systems in selected countries, found that even as the top-ranked country, Australia does not do well on measures of access and care process (a domain that includes prevention, safety, coordination, patient engagement and preferences).
Common themes, common conclusions
No matter whether government, clinical, researcher or community-driven, there are common themes across these reports. All describe the impact of the social determinants of health and surges in long-term conditions and mental health needs, particularly among children and young people. All describe systemic failures.
All convey a mixed picture of the quality and experience of care and variations in equity of access to care. All refer to the need to adjust where health budgets are spent.
All conclude that if we don’t remedy and transform primary care, not only will the sustainability of our health systems suffer so, too, will the productivity, prosperity and wellbeing of nations.
Seven prescriptions for impact
In this vodcast, three global experts discuss their ‘top pick’ prescriptions for change.
The power of data
"Data is something we really need to get in order ….Data is our guide for equity and quality care. When we don’t have that, we lose out on the opportunity to lean into what our patients and communities really need for their health."
Dr Kirsten Meisinger, Director of Leadership and System Transformation, Harvard Medical School Centre for Primary Care
Data supports population health management by tracking and analysing health outcomes, identifying gaps in care, and developing targeted interventions. Predictive analytics assists in decision-making, identifies patients at high risk of readmission or complications, allows providers to intervene early, and prevents adverse outcomes. If we are to harness the power of data, this needs to happen at the national, regional and service level through infrastructure that can share data across different platforms and settings, investments in the necessary technology, and education to ensure that staff are trained to use it effectively.
From analogue to digital
"We have to stop thinking about tomorrow‘s health systems with a mindset of today’s technology. Tomorrow’s technology is going to be exponentially better than today’s."
Dr Paresh Dawda, Founder and Director, Prestantia Health
Health systems must transition from analogue to digital to improve efficiency, accuracy, and patient outcomes. Digital systems such as electronic health records streamline processes, reduce paperwork and errors, while enabling quicker access to patient records and real-time data. This enhances decision-making, improves coordination among providers, and reduces duplication of tests and procedures. Digital platforms also facilitate telemedicine and expand access to care. They enable better data collection and analysis, helping healthcare systems track trends, manage resources, and improve overall care quality.
Care closer to home: neighbourhood approaches
“The 21st century is the century of systems. Every system requires a network to deliver the change….We must back our primary care networks.”
Dr Johnny Marshall, OBE, National Association for Primary Care, UK
Poor health is more evident in socio-economically deprived communities and some population groups. To reduce disparity, we need to empower communities to take charge to have agency over the kind of care they can access. Communities must be able to self-design their own healthcare as well as shape health-creating infrastructure such as libraries and green spaces. This means devolving power to local leaders who have the permissions, governance, funding and infrastructure to mobilise services across the entire local health and care ecosystem to deliver what is appropriate close to home. This means a fundamental role for regional organisations such as Australian Primary Health Networks working in place-based collaborations.
Rethink health care destinations
“Where are people interacting with health care? Wellness, supermarkets, wearables. We have responsibility to embrace the use of health care settings that are beyond what we think of traditional healthcare because our patients have moved ahead of us.”
Dr Kirsten Meisinger, Director of Leadership and System Transformation, Harvard Medical School Centre for Primary Care
Findings that less than half of Australian adults have a longstanding relationship with a primary care provider is concerning and a trend evident in many other countries. Yet shifts beyond the "one doctor, one patient, in clinic" paradigm is important to foster a collaborative, team-based approach to healthcare. Moreover, 10% of a practice’s population generally requires 50% of its time – a striking fact that reinforces the need for this approach to ensure that no aspect of a patient’s care is overlooked. People that take up the most time have complex health and social care needs that demand a wide array of skills, drawing not only on general practice, nurses, multiple specialists and allied health professionals but also social, aged and mental health care workforces.
Real teams activated around a common purpose
“We have to build real teams in the communities that are matched to the health and wellbeing needs of the very communities we serve….to work with the communities to re-imagine what the care and support offer might be, build skills into the functions of those teams and have the necessary ongoing training, support and evaluation.”
Dr Johnny Marshall, OBE, National Association for Primary Care UK
The future of health care lies in creating flourishing, multidisciplinary teams. Effective teams need to galvanise around a common purpose, deliver together, continuously evaluating their efforts and practise compassionate leadership in a team climate of trust and psychological safety. This kind of collaboration requires the right regulatory and financial enablers but also investment at the service level to not only development leadership skills among community-based teams to redesign their care models and oversee change, to bring others along with them.
Leadership and distributed ‘new’ power
“We have to invest in leadership skills within our front-line staff working with the populations they know and then activating the whole workforce so that we understand we all have a role in delivering with our communities together”
Dr Johnny Marshall, OBE, National Association for Primary Care UK
Leadership should not confined to the executive level. It needs to extend to clinical leaders, frontline staff and consumers. There is enormous scope to better utilise the skills of the various actors in health care systems not only in terms of how their clinical care skills can be optimally harnessed to prioritise patient outcomes, but also to champion a culture of continuous improvement, and serve as agents for innovation and collaboration across different levels of organisations and systems. Health system leadership must also include serious investment in consumer leadership. Consumer insights improve services, experiences and outcomes: consumers and carers can help us see tomorrow. Policymakers, administration and clinicians must learn new ways to harness the transformative role consumers can play as agents of change.
Health creation
“The health care sector is quite reactionary and specialist dominated, and we think of things in problem-lists. Patients, who are actually people, think of themselves as whole beings. If we can’t move our paradigm into that mindset then we are going to become increasingly marginalised and irrelevant”
Dr Kirsten Meisinger, Director of Leadership and System Transformation, Harvard Medical School Centre for Primary Care
Care that creates health and wellbeing through health promotion and prevention action must be a cornerstone of future primary care delivery, supported by advanced analytics that predict health risks and suggest timely interventions, providers focussed on prevention through regular screening, lifestyle counselling, social prescribing and community-based health promotion programs.
Outside the walls
“Tomorrow belongs to those who can hear it coming”.
David Bowie
When you can forecast the future, you can do something about it. In imagining a better health care future, there are aspects we shouldn’t change: relational compassionate care must remain the constant, but everything else is up for disruption.
Think tanks have long described the over-reliance on hospital care and the political reluctance to challenge this as a barrier to change in health systems.
Policymakers acknowledge system interdependencies, particularly that hospitals will only be able to manage demand by working in different ways, including delivering more care beyond hospital walls.
It’s time to start taking primary care outside of its traditional walls too. It’s time to conceive of primary care as something wider and more community connected.
“It’s about co-production and working together with people to meet them where they are in order to deliver their care. It’s about not being bound by boundaries. Health care doesn’t necessarily happen in general practices, clinics and hospitals, it happens in communities neighbourhoods and where people go”
Dr Paresh Dawda, Founder and Director, Prestantia Health
Just as the system is complex, so are the solutions. But just as general practices can embrace improvement and innovation by breaking down the steps for change and taking a ‘plan, do, study, act’ mindset, so too can the system.
Primary care is where we most need transformation and investment, and we have the knowledge and levers to accelerate change.
Accelerating action on these seven prescriptions would start to shift the dial toward ideal health care.




Comments