Beyond engagement: consumers and communities as agents of health care change and improvement
- Leanne Wells

- May 2, 2025
- 8 min read
Updated: May 2, 2025
Leanne Wells and Paresh Dawda
The first vodcast in the Australian Primary Health Care Insights and Innovation Series highlighted that health system leadership must include consumer and community leadership. Harnessed and supported in the right way, consumer insights and preferences improve policies, services, experiences and outcomes.
Embracing new ways
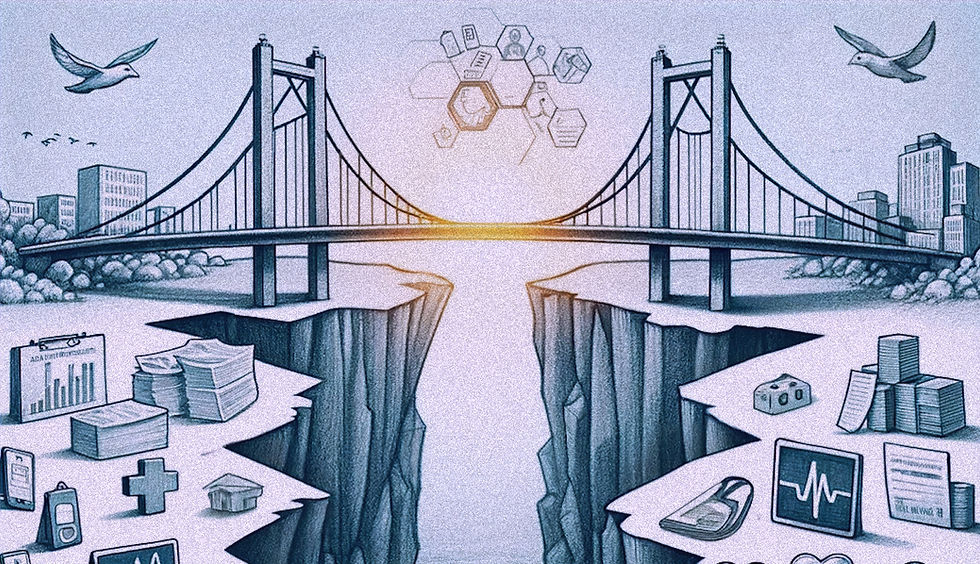
Policymakers, health administrators and clinicians must learn and embrace new ways to harness the transformative role consumers, community members and carers can play. Conversely, consumers and communities need support, capability and capacity to engage as equals in policy, research, program and service design. This is necessary if our governments are to be less technocratic and realise the vision where all members of society can live the best life possible.
If we are to realise the Productivity Commission’s vision that “all Australian Governments should re-configure the health system around the principles of patient-centred care”, such practices need to be reinforced by health systems and governance arrangements that ensure that systemic, strategic consumer and community engagement is a ubiquitous and valued part of the way health systems function.
“Healthcare is there to serve the people, it’s there to improve the wellbeing and the lives of people who are patients within that system. All too often those people don’t have a voice in how the system is designed and too many other people have the power within the system to shape it"
Dr. Tara Kiran, Family Physician and Scientist, St Michaels Hospital, Unity Health Toronto and Fidani Chair in Improvement and Innovation, University of Toronto
As developed countries grapple with sustainability and how best to assure and strengthen primary health care, it is important that our system leaders and those who translate policy into services build trust by developing and demonstrating that they have a firm grasp on consumer and community expectations and preferences.
“Health is about delivering public value and you can't deliver public value without involving the public”
Dr Paresh Dawda, GP lead and adviser. Founder, Prestantia Health
A strong and developing tradition
Our system already features many ways to support consumer and community involvement. There are formal processes, including Royal Commissions, parliamentary inquiries, and government-led consultations. The Australian Commission for Safety and Quality in Healthcare mandates a partnering with consumer standard against which all hospitals are accredited. Primary Health Networks (PHNs) are required to have a community advisory committee as part of their governance structures, and it is commonplace for local hospital networks to have some form of consumer engagement forum.
The consumer and carer movement has largely been championed by mental health sector largely commencing with the Mental Health Statement of Rights and Responsibilities in 1991 and culminating decades later with government recognition and funding for two independent national peak bodies, one for mental health consumers, the other for carers. In addition, the Consumers Health Forum of Australia serves as the national longstanding peak body representing consumer’s health interests. In a speech to a CHF event not long after its establishment in 1987 the then Health Minister the Hon Neal Blewett said:
“Without informed, knowledgeable and articulate health consumers, health policy will always be unbalanced whatever the goodwill and idealism of governments and health providers. Mature consumer organisations are an essential part of the health equation.”
Involve the public to deliver public value of health care
To further elevate and underscore the importance of consumer and community involvement, the World Health Organisation (WHO) has produced a social participation declaration. It too recognises that lived experience and knowledge shapes better policy, more inclusive health systems, improved services, experiences and outcomes. It also recognises that while people are increasingly being engaged as partners in health systems, recognition and influence is variable. Most importantly, the resolution makes social participation a core function within health systems, committing countries to strengthening, systematising and sustaining social participation.
Formal, institutionalised, organisational pathways for consumer and community involvement have their place, but are they enough? Writing about the declaration Canadian patient advocate, Vincent Dumez, and colleagues and their vision for the practices that should ensue summed it up well when they said, “let’s amplify people’s voices by connecting grassroots to the treetops”.
It's true that the health system is constantly learning and improving. Where might we look for improvement and excellence in consumer and community involvement?
A Sydney Policy Lab report calls for greater engagement with policy makers through strengthened forward-looking, collaborative policy development that is led by the communities and the people whose lives and livelihoods are most at stake to help tackle the serious global and domestic challenges we face as a nation.
Exemplars of social participation in action
The Lab has actively explored the potential deliberative democratic methods used with increasing frequency in key OECD countries through formats such as citizens’ assemblies, juries and panels. The Lab’s aspiration is for “members of the public to write their own agenda for care, deliberate over relevant evidence, and determine key priorities for the future of care policy, thereby improving outcomes and, in turn, strengthening our democracy”.
We have seen such processes start to emerge and mature in health care.
The OurCare initiative led by Dr Tara Kiran is the largest pan-Canadian conversation about the future of primary care. It is a prime example of a systematic multi-pronged, iterative, deliberative, inclusive community engagement effort with the sole purpose of shaping change in health care policy.
OurCare engaged almost 10,000 people about their experiences of primary care and their values, ideas, and hopes for the future of that care. The conversation placed special emphasis on reaching people who have the greatest needs of care, face the greatest barriers to accessing care, and are most likely to be excluded from policy-making decisions about primary care.
“The primary care system in Canada is widely regarded as being in crisis right now. The reason we started OurCare is because we wanted to bring that public voice into the discussion of what these reforms should look like. What should the vision for primary care be like moving forward? What are the pain points and what are the priorities that the public have?
Dr. Tara Kiran, Family Physician and Scientist, St Michaels Hospital, Unity Health Toronto and Fidani Chair in Improvement and Innovation, University of Toronto
The approach involved:
A National Survey of over 9,000 people exploring access to care, what matters most to people, service utilisation and experience, health records and options for system redesign,
Provincial Priorities Panels which engaged people in deep dialogues about primary care. Participants who were randomly selected to match the demographics of the province, learned from primary care experts and then deliberated in small groups to reach consensus on values that should underlie the primary care system and recommendations for a better system, and
Community Roundtables involving people consistently underserved by primary care including First Nation, Inuit and Metis Peoples, Newcomers, Members of the Black Community, the LGBTQIA+ community and people with disabilities to generate their values and recommendations.
“The third phase was designed to amplify voices we missed in the first and second phases. We really tried hard to have diversity and partnered with community organisations that had established relationships with members of marginalised communities”
Dr. Tara Kiran, Family Physician and Scientist, St Michaels Hospital, Unity Health Toronto and Fidani Chair in Improvement and Innovation, University of Toronto
The ultimate output was the OurCare Standard which presented a bold vision for the future of primary care in Canada: a vision centred on the values and priorities of patients and the public, and intended to serve as a vision that policymakers, clinicians healthcare administrators and researchers and others can all agree on and use as a basis for change.
“The OurCare standard is six simple statements that define what every person in Canada should be able to expect from the primary care system. Those statements have garnered a lot of traction from our policy makers and are starting to be taken up as really the direction we need to go when we are thinking about reform in our country”
Dr. Tara Kiran, Family Physician and Scientist, St Michaels Hospital, Unity Health Toronto and Fidani Chair in Improvement and Innovation, University of Toronto
The Standard and the reports generated throughout the OurCare Initiative have stimulated considerable interest from policy makers, ongoing community conversations and media coverage of the need for a better primary care system in Canada.
“Health professional groups get a lot of time with government. They have a lot of power in the system. There are many others with financial interests. People have gravitated to the work we've done because we amplified the voices of the public and everybody agrees that the system is there to serve patients and the public.”
Dr. Tara Kiran, Family Physician and Scientist, St Michaels Hospital, Unity Health Toronto and Fidani Chair in Improvement and Innovation, University of Toronto
Closer to home, a more localised model of consumer and community engagement has been introduced in Western Sydney where Wentwest provided funding to set primary health and social care priorities using a deliberative democratic participatory approach in the form of two citizens’ juries.
Publicly funded primary health care investments by Primary Health Networks are usually informed by analysis of locally collected data, surveys, focus groups and consultations. Western Sydney wanted a more ambitious approach to a deeper understanding of baseline health and social care priorities in their culturally diverse footprint.
“The idea of getting system wide input from people is powerful. It’s good to get ideas from the data, but it's often not the case that you're hearing from the community about what they particularly want or need. What I've seen over the years is that the people that hold the power will come in and they'll say: what do you think about what we think instead of what do you think? ”
Dr Coralie Wales OAM, Honorary Community Fellow, Western Sydney University
The juries involved transcribed facilitated discussions with a diverse, representative group of Western Sydney citizens. Practical support for the jurors included oversight by the Wentwest Consumer and Clinical Advisory Councils, internal and external advisory groups, expert presenters and a handbook. Four consumer advisors were included in the research team.
“We had to find a question - that is an important part. Over a couple of months of thinking, talking and listening, we decided to ask the question: should we, the people of Western Sydney, continue to invest in the health system in the same way as we have in the past?”
Dr Coralie Wales OAM, Honorary Community Fellow, Western Sydney University
The juries reached consensus on a set of recommendations for primary care investment. These included support for a greater focus on prevention, including early intervention to keep children thriving and connected at school, and better cross‐sectoral bonds via coalitions to enable social care to be linked to health care. Team‐based care in general practice and building a culture for relationship‐based care, proactive data use and developing a patient‐centred workforce through incentivising students and expediting registration of overseas trained health workers were recommended.
The use of citizens’ juries in primary health settings is rare, and the Western Sydney experience has given Wentwest and its implementation and research team a solid understanding of what investments will deliver and has spurred the organisation to continuing this deliberative approach in a permanent citizens’ assembly.
More broadly, the Western Sydney experience suggests that inclusive methods for effective consumer and community engagement such as deliberative citizen juries can be useful tools in a primary health care setting. This is particularly the case for PHNs who are charged with commissioning services and supporting primary care solutions to better serve the diverse and complex needs across varying Australian geographies.
The Canadian and Western Sydney case studies illustrate the dictum that change won’t happen unless the right people – citizens - tell the right people – governments and policy makers - it is needed.
“We need to do more of these kinds of approaches: scale it, share, learn from it. We need microsystems and organisations like PHNs to do this on a regular, frequent basis and aggregate that information upwards to stimulate policy”
Dr Paresh Dawda, GP lead and adviser. Founder, Prestantia Health
‘‘We know the future of health and care can’t just be designed in boardrooms. Real change happens when communities lead, when local voices are heard, and when the people closest to the challenges are the ones shaping the solutions”.
UK Kings Fund
This blog and accompanying vodcast is the third in the Australian Primary Health Care Insights and Innovation Series hosted by Prestantia Health and AUDIENCED. Watch our website for future installments to the series.
For more information about OurCare, visit OurCare.ca and subscribe to the podcast Primary Focus with Dr. Tara Kiran wherever you get your podcasts.
.




Comments